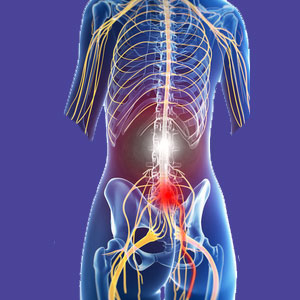
Lumbar foraminal stenosis describes a reduction in patency in the openings through which the spinal nerve roots travel in the lower back. Foraminal stenosis is a normal part of aging and is directly facilitated by other spinal degenerative processes, such as intervertebral disc desiccation and osteoarthritis. Foraminal stenosis is not painful, but can create problems if the nerve contained within the narrowed foraminal space is compressed.
The lumbar nerve roots are the major source of lower back pain, with more diagnoses enacting pain through structural compression of these tissues than through any other causative mechanism. That being said, the foramina in the lumbar spine are usually still large enough to prevent compressive neuropathy conditions from occurring, even when markedly severe degeneration occurs.
This important dialog provides a truly objective look at narrowing of the lumbar foraminal openings. We will examine why these spaces tend to fill with arthritic material, as well as what symptoms might exist when the nerve is verifiably impinged upon. Finally, we will provide some important details on why foraminal stenosis is one of the most often misdiagnosed sources of lower back pain.
Lumbar Foraminal Stenosis Causes
Foraminal stenosis is normal to experience and nowhere in the spine is it more prevalent than between L4 and S1. In most adults, foraminal narrowing will be markedly present during their later 30s, with many people displaying reduction in patency even younger. Therefore, there really is no direct cause of foraminal stenosis in many patients, except for age and activity-related alterations that are considered totally normal parts of getting older.
Disc desiccation begins the process of foraminal narrowing in most people, since this process occurs relatively early in life and brings the lumbar vertebrae closer to one another. As the bones become closer, the space through which the nerve root passes out of the spine shrinks. Disc desiccation also facilitates the lumbar spinal osteoarthritic processes, which also tend to act on reducing the patency of the neural foramen. Many people experience an accumulation of arthritic debris and bone spurring in and around the foramina due to facet joint and general structural deterioration.
Other spinal irregularities can contribute or directly cause narrow neural foramen as well, with the most common being scoliosis, lordotic changes, spondylolisthesis, ligamentous abnormalities, herniated discs and various congenital conditions. Injury can cause or contribute to neural foraminal narrowing acutely or by inciting the degenerative processes to accelerate in specific areas of the vertebral anatomy.
Foraminal Stenosis Symptoms
Foraminal stenosis is not inherently symptomatic in any way. It is merely a typical aspect of aging. The vast majority of cases observed at any given vertebral level will not be symptomatic. However, if the nerve root contained within the foramina becomes compressed, then symptoms are likely to occur and might be quite severe. Therefore, we will detail the symptoms of a compressive neuropathy that may be created by severe foraminal stenosis:
Pinched nerves are greatly misunderstood and are not typically the source of chronic pain. Pinched nerves generate symptoms because nerve signals do not transmit correctly and eventually will not transmit at all. Pain might be a temporary expression, along with tingling and a burning sensation in the innervated region of the body or at the local site of compression. However, this pain will fade quickly to be replaced by numbness and weakness in the innervated area of the body and possible physical dysfunction.
Symptoms in innervated regions should correspond to nerve conduction studies and nerve mapping charts. Symptoms that appear illogically elsewhere in non-innervated areas should never be linked to a compressive neuropathy. This seems like common sense, but does not prevent mistaken diagnosis from affecting millions of patients yearly, even when the symptoms do not correlate at all to the clinical expectations for location and/or expression.
Lumbar Foraminal Stenosis as a Diagnosis
Diagnosing lumbar foraminal stenosis is controversial, since it is basically now known to be a universally-experienced part of aging. We tend to agree that the diagnosis can impart a horrific nocebo effect and is often poorly understood by patients. Both of these negative factors can be escalated by opportunistic care providers who prey on ignorance and will use the chance to convince the patient that they need treatment, often without any scientific evidence or merit.
Severe foraminal stenosis should be monitored, but not treated, unless the patient is definitively experiencing logical symptoms that correlate and can be further investigated to verify their source. The vast majority of people who are labeled with a diagnosis of foraminal stenosis demonstrate the exact same age-related changes that are commonplace in every human adult and provide no proof that any back pain, which may be present, is definitely linked to the impingement of a particular spinal nerve. In fact, almost all diagnosed patients, who have pain, experience symptoms which are far too widespread and diverse to ever possibly come about as a result of a single level compressive neuropathy. This is proven scientific fact.
Lower Back Pain > Causes of Lower Back Pain > Lumbar Foraminal Stenosis





